For the funds with automatic pre-benefit screening, a Personal Declaration of Health is completed when a person is employed and therefore it is possible that they will be sent prior to the processing of the payroll.
These forms therefore need to be able to be linked to a Service Request and then the Service Request merged with the one created via the underwriting batch job (BJU3AZ).
An email box must be set up for the above process. The scheme parameter EMAIL is currently part of the system configuration. The user will not have access as it contains usernames and passwords.
A Service Request must also be created if the Personal Declaration of Health is received via fax or post before the Underwriting batch job has created a Service Request and a Membership Risk Cover record on which the document can be loaded.
The Service can be Pended with a Pend Reason of MEMBER NOT FOUND.
When a Service Request is created manually i.e. the My Work > Service Request > Create option is selected on the JU7AB Work Management List screen and the Process selected is PRE-BENEFIT SCREENING, the Activity will default to RECEIVE MEDICAL.FORM.
When the existing polar program accesses the PRESCREENING email box, a Service Request will be created for each email with the following detail:
- Scheme Code linked to the email box
- Process Name: PRE-BENEFIT SCREENING
- Activity Name: RECEIVE MEDICAL FORM
- Status: OPEN
All of the attachments on the email will be attached to the Service Request.
When the Service Request is indexed, the system will check if there is an existing Service Request with the same Scheme Code, Reference Number and Process. If there is, the system will provide an informational message to indicate that it already exists and it will be merged with the existing Service Request. If there is more than one Service Request, the system will merge the Service Request to the Service Request with the earliest Timestamp.
Note:
A member with a Status of MERGE or INACTIVE may not be used as a member for Indexing purposes.
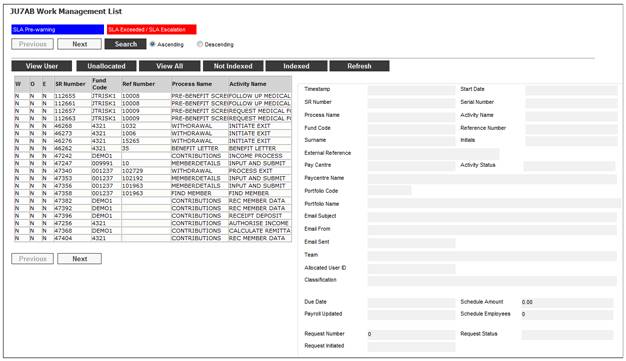
When you select my work from the system functionality menu, the JU7AB Work Management List screen will be displayed.
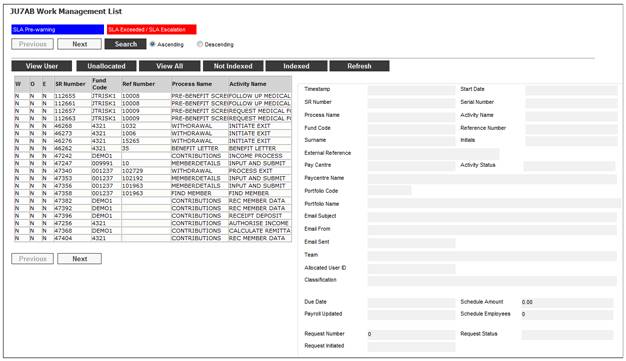
This screen displays a list of the service requests allocated to you.
For detailed information on the JU7AB Work Management List screen and the functionality of the action buttons refer to
My Work
Service Requests
Highlight the Pre-Benefit Screening or Underwriting Service Request on the JU7AB Work Management List screen, and then select Service Request > Process from the sub-menu on the left.

The JU3BL Membership Risk Cover screen will be displayed.
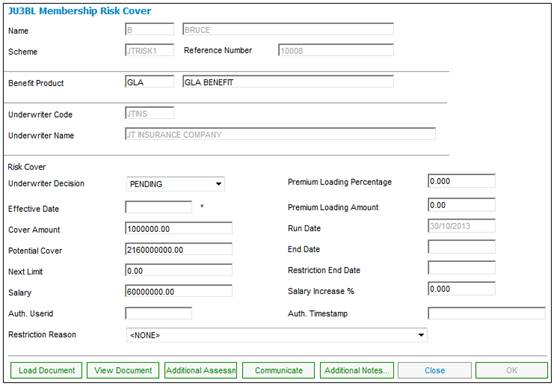
View Document
When the VIEW DOCUMENT button is selected, the documents linked to the JU3BL Membership Risk Cover record will be displayed. Only users with the necessary access linked to a Document Category equal to UNDERWRITING will have access to view the documents.
If no documentation has been received or further documents are required, the COMMUNICATE button must be selected.
Communicate
When the COMMUNICATE button is selected, the system will flow to the JU3BN Membership Risk Cover Communication screen.
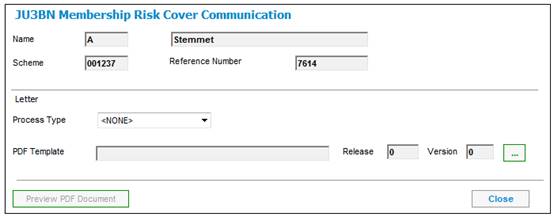
Select PRE SCREENING or UNDERWRITING from the Process Type drop-down list and click the LIST button for the PDF Template field.
The JU3BN Letter Template List screen will be displayed.
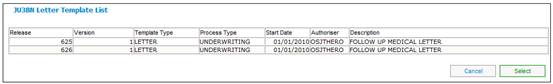
This screen lists the Document Templates with a PDF Process of PRESCREENING or UNDERWRITING.
Highlight a Template and click SELECT. The JU3BN Membership Risk Cover Communication screen will be displayed with the selected Template. Click the PREVIEW PDF DOCUMENT button to display the document.
Close
When the CLOSE button has been selected, the Process Flow screen will be displayed.
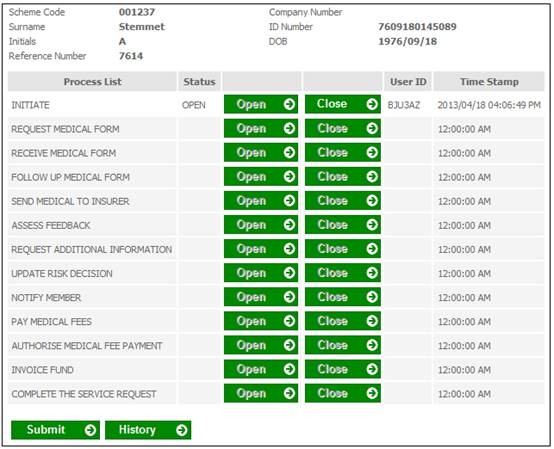
Select the next Activity Name that the Service Request must be updated to. When the SUBMIT button is selected on the Process Flow screen, the system will flow back to the JU3BL Membership Risk Cover screen for the next action to be performed.
When the button for SEND MEDICAL TO INSURER is selected in the Process List column on the Process Flow screen, the system will flow to the JU3BL Membership Risk Cover screen from where the COMMUNICATE button can be selected to select the relevant templates for the information to be forwarded.
If the Status of a Service Request is PEND due to information outstanding and is processed before the number of days on the JU7AB Create/Update New Service Request screen has expired, the Process Status on the Service Request will be updated to OPEN.
Note:
In some cases a Service Request Activity Name must to be updated again with an Activity Name that was previously completed on the Process Flow screen e.g. if the button for REQUEST ADDITIONAL INFORMATION has been selected in the Process List column on the Process Flow screen, then a previous item FOLLOW UP MEDICAL FORM may be required to be selected if the additional requirements haven’t been received. This can be achieved by selecting the OPEN button for the particular item that needs to be selected again.
Similarly it is possible to close multiple items at the same time e.g. if the documents are received without requiring follow up then the Followed up on Outstanding Medical Requirements can be closed and the next Activity Name on the Process Flow screen will be opened.
Activity Name: INITIATE
When the BJU3AZ Underwriting batch job runs and the Members’ insured cover or salary is checked to the Evidence of Health (EOH) Limit for a Benefit Product linked to the INSURED Benefit Package for the Membership Group to which the Member is linked, and a Membership Risk Cover record has been created, the system will insert a Service Request on My Work with a Process Name of UNDERWRITING with an Activity Name of INITIATE. The Start Date will be equal to the Effective Date on the Membership Risk Cover record and with the Scheme Code and Membership Reference Number.
Activity Name: SEND MEDICAL TO INSURER
When the SEND MEDICAL TO INSURER button is selected on the Process Flow screen, the system will flow to the Membership Risk Cover screen from where the COMMUNICATE button can be selected to select the relevant templates for the information to be forwarded.
If the Status of a Service Request is PEND due to information outstanding and is processed before the number of days on the JU7AB Create/Update New Service Request screen has expired, the system will update the Process Status on the Service Request to OPEN.
Activity Name: FOLLOW UP MEDICAL FORM
In some cases a Service Request Activity Name needs to be updated again with an Activity Name that was previously completed on the Process Flow screen e.g. if the Request Additional Information item has been completed then a previous item FOLLOW UP MEDICAL FORM may be required to be selected if the additional requirements haven’t been received. This can be achieved by selecting the OPEN button for the particular item that needs to be selected again.
Activity Name: ASSESS FEEDBACK
When a Service Request with an Activity Name of ASSESS FEEDBACK is processed, the system will flow to the JU3BL Membership Risk Cover screen from where the VIEW DOCUMENT button can be selected to review to Underwriter feedback.
Activity Name: UPDATE RISK DECISION
When a Service Request with an Activity Name of UPDATE RISK DECISION is processed, the system will flow to the applicable Membership Risk Cover screen. The decision can then be recorded by selecting a value of ACCEPTED or DECLINED from the drop down list for Underwriter Decision.
If the value of ACCEPTED is selected and a restriction on the cover amount is to be applied then the restricted cover amount must be captured in the Cover Amount field.
Activity Name: PAY MEDICAL FEES
When a Service Request with an Activity Name of PAY MEDICAL FEES is processed, the system will flow to the JU2BK Accounting Journal Details screen from where a payment will be captured. When the OK button is selected, the Activity Name of the Service Request will be updated to AUTHORISE MEDICAL FEE PAYMENT. The system will flow back to the My Work 7AB Management List screen.
When the Service Request is processed, the system will flow to the JU2BK Accounting Journal Details screen from where a payment will be authorised. When the OK button is selected, the Activity Name of the Service Request will be updated to the next item on the Process Flow screen. When the Service Request is processed, the system will flow back to the Membership Risk Cover screen from where the next action can be performed.
Activity Name: AUTHORISE MEDICAL FEE PAYMENT
When the Service Request is processed, the system will flow to the JU2BK Accounting Journal Details screen from where a payment will be authorised.
When the OK button is selected, the Activity Name of the Service Request will be updated to the next item on the Process Flow screen.
When the Service Request is processed, the system will flow back to the Membership Risk Cover screen from where the next action can be performed.
Activity Name: INVOICE FUND
When a Service Request with an Activity Name of INVOICE FUND is selected, the system will flow to the Claim Assessment screen from where the COMMUNICATE button can be selected for the relevant template to be selected for correspondence to be forwarded to the Fund.
Activity Name: COMPLETE THE SERVICE REQUEST
When the CLOSE button is selected on the Process Flow screen for the Activity Name COMPLETE THE SERVICE REQUEST, the following message will be displayed:
This will complete ALL processing and finalize the Service Request.
Are you sure you want to Finalize?
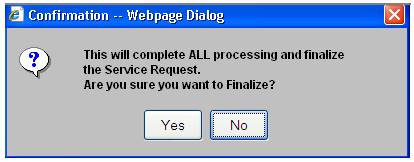
Click YES to update the Service Request Process Status to COMPLETED.
Click NO to remain on the Process Flow screen from where the next Activity Name can be selected.
For more information refer to
Clients
Underwriting
Supplements
Processes
Underwriting